MECHANISM OF PROTEIN PRESERVATION IN BONE AND BLOOD VESSEL WALL
This is the mechanism of protein preservation in bone and blood vessel wall.
The story behind Vitamin K2.
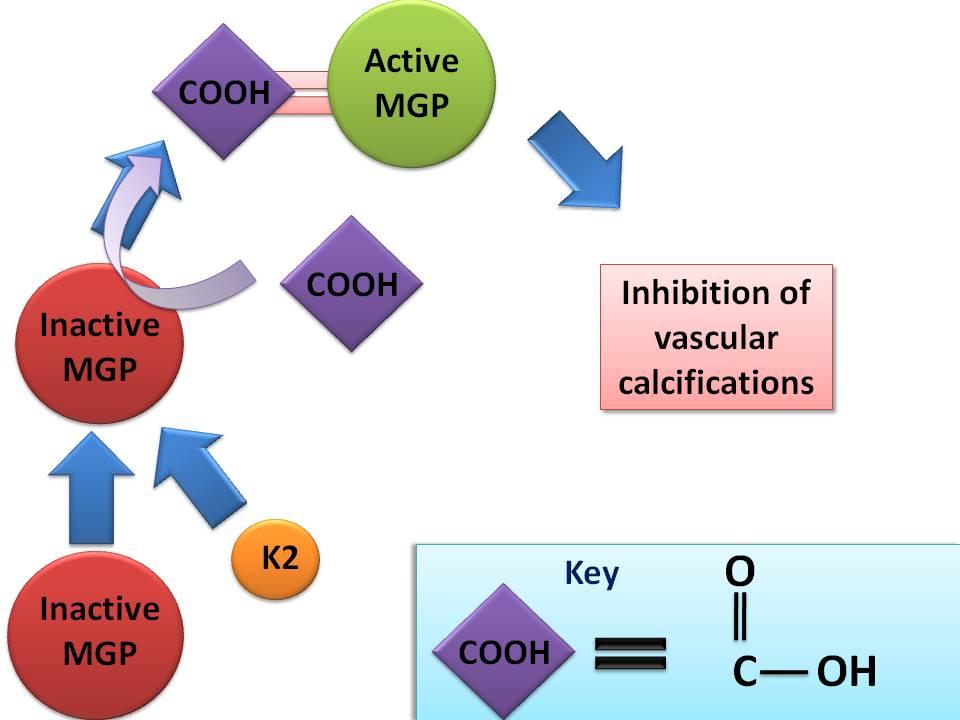
Vitamin K2 inhibits vascular calcifications by means of a Vitamin K dependent protein called matrix-Gla-protein (MGP). MGP is produced by osteoclasts, chondrocytes, and the vascular smooth muscles of the arterial walls.
Mutant MGP genes cause calcifications of the aorta, coronary, and cerebral arteries. Moreover, in rodents, Vitamin K can be inhibited by Coumadin (warfarin) which is a blood thinner. Vitamin K deficiency results in vascular calcifications which can be prevented by Vitamin K2 but NOT Vitamin K1.
In order, for MPG to become activated, there must be sufficient Vitamin K2 to allow for "carboxlyation" or addition of a COOH group to MPG. (see above)
The two commercial forms of Vitamin K2 are MK-4 (half life of 1 hour) and MK-7 (half life of 3 days). I have no interest any specific products but I did find Super K with Advanced K2 Complex from Life Extension containing: MK-4 1000 mcg, MK-7 100 mcg, and Vitamin K1 1000 mcg. A more natural form would be Butter Oil which is more expensive, or Japanese fermented soybeans called Natto.
Now for a look at some studies.
Knapen, et al randomized 325 postmenopausal women ages 55 to 75 years into two arms - placebo vs 45 mg per day of MK-4. MK-4 did not affect bone mineral density but did have a positive affect on bone mineral content and the femoral neck width in relationship to placebo. Hip bone strength remained unchanged in the MK-4 group during the 3-year trial period, whereas in the placebo group bone strength decreased significantly. Compact, bending, and impact strength indices were more preserved in the Vitamin K2 group.
A study in the Journal of Nutrition took 4807 Dutch men and women 55 years of age and over and revealed that Vitamin K1 had no statistical impact of aortic calcifications, coronary heart disease, or non-fatal myocardial infarctions (MI). Whereas, lower intakes of Vitamin K2 was associated with a higher risk of non-fatal MIs, coronary artery disease, and severe aortic calcifications.
A Japanese study in rats has shown that long-term warfarin (Coumadin) therapy weakens rib and vertebra by decreasing bone osteocalcin content but did not reduce hip strength. Hip strength was not reduced due to compensatory strengthening during ambulation. Long term warfarin did not change bone mineral density.


